 The sooner you call, the more effectively we can enhance the quality of life for both the patient and family. Our staff is available to help determine when a patient can benefit most from hospice or palliative care. If you received palliative care in the hospital we can continue those services at home.
The sooner you call, the more effectively we can enhance the quality of life for both the patient and family. Our staff is available to help determine when a patient can benefit most from hospice or palliative care. If you received palliative care in the hospital we can continue those services at home.
When you call us, you can expect to speak with a nurse to discuss your goals of care and needs. Together we can identify a care plan to help you meet those goals. We walk you through the process and help you to feel comfortable with each step. Your questions and input only make us better able to help, so please feel free to ask questions an make your requests known.
“As a nurse with Allumine Hospice, I appreciate our specialized care. I appreciate being able to walk the journey with each patient and show them that the time we spend is not about their death, but rather about living as completely as possible with each day we have. I have time to spend with each patient and am able to help them accomplish little goals along the way. I love what I do and wish that people were less afraid. I hope that I can be a light in the darkness, and I believe that is truly the mission of Allumine Hospice.”
Available 24/7 and we encourage you to call us with any questions or concerns.
Able to anticipate symptoms and alleviate them before they become severe.
Will prevent you from spending your time in a hospital setting.
Experienced and committed to excellence.
Accept Medicare, Medicaid, and most major insurances.
We Honor Veterans
America’s Veterans have done everything asked of them in their mission to serve our country. Allumine Health believes it is never too late to give them a hero’s welcome home. That’s why Allumine Hospice caregivers are on a mission to serve those who have served us.
As We Honor Veterans Partners we are committed to
- Learning about the unique needs of Veterans and their families
- Educating our staff and communities about caring for Veterans facing serious illness
- Coordinating care with VA and other healthcare organizations
- Providing Veteran-to-Veteran volunteer programs
- Delivering the best quality health care We Honor Veterans Partners can help Veterans and their families to: Enroll and access VA benefits Be recognized for their service with special ceremonies Replace lost medals and awards Receive extra support from other Veterans
Resources
Frequently Asked Questions
Hospice care provides comfort and kindness to those persons near the end of life’s journey. Hospice will help you make decisions about how and where you want to spend the rest of your life. Hospice is about living well until the end of life. Hospice neither hastens nor postpones death. It is a life-enhancing support system that promotes the best quality of life for the patient and his or her family. It enables the patient to remain at home and caregivers to receive instruction and support in caring for their loved one.
Hospice treats you, not the disease. The focus is on care, not cure. You and your family’s medical, social, emotional, and spiritual needs are addressed by a team of hospice professionals and volunteers. Hospice will provide comfort care when cure is no longer an option. Through ever advancing technology, pain and symptom control will enable you to live as fully and comfortably as possible.
Hospice considers your entire family, not just you as the “unit of care.” You and your family are included in the decision-making process. Hospice will help you and your family make choice about end-of-life issues and enable you to have greater control over these choices. Bereavement counseling is also provided to your family for up to 13 months after your death to ensure that they are cared for too.
It means that instead of focusing on curing the disease it may be best to focus on helping the patient live as fully as possible. Hospice is intended for patients with a life expectancy of six months or less, but no one is able to accurately predict how long someone will live. Hospice is started to better meet the needs and goals of the patient.
We believe the best way to discuss hospice care is to begin by listening. We would like to speak with you directly. You can call us 24/7 to discuss any questions you or your loved one may have about enrolling in hospice care. We truly desire to walk with you through this journey. Please never hesitate to call us.
When the burden of treatment outweighs the benefits and/or the patient has had multiple hospitalizations over the last several months, he/she might be ready for hospice. You may consider:
- Repeat trips to the Emergency Department
- Unrelieved pain
- Frequent Infections
- Sudden or progressive decline in physical functioning and eating
- Weight loss/difficulty swallowing
- Shortness of breath/increased oxygen dependence
A patient is eligible to receive hospice services when their illness is terminal, meaning a physician has determined that they could die within six months if the disease continues as expected. There are medical guidelines that accord with the patient’s disease and help a physician make a hospice referral.
We provide hospice care in the place a patient calls home. We are able to help you keep a family member in a private residence and also partner with many area facilities including assisted living facilities, skilled nursing facilities, and local hospitals to provide care and services.
Every patient and family is assigned a Case Manager. The Case Manager is an experienced nurse trained to help you navigate healthcare at the end of life. Your Case Manager will keep you informed of scheduled visits during the week by each team member and will be your contact to ensure all of your needs are met and that we are working to assist you in meeting your goals and wishes.
The hospice nurse creates a plan of care with your input, designed to meet the patient’s needs. This determines the frequency of visits by the doctor, nurse, social worker, chaplain, aide, and therapists you may need.
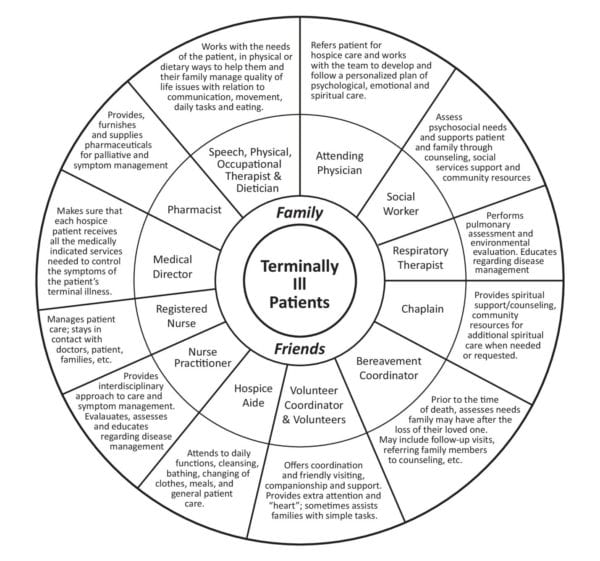
Allumine Hospice Team
Registered Nurse Case Manager: You will be assigned a Registered Nurse Case Manager who will coordinate your care with other members of the interdisciplinary team and handle any nursing needs. The role of the nurse is to help prevent and relieve pain and other symptoms, and to teach caregivers ways to provide your care. The nurse will make certain that necessary medical supplies and equipment are ordered and will assist in monitoring medications. Regular communication with your physician will make certain that he/she is aware of your status and that orders are being followed. Your hospice nurse will try to anticipate your needs and assist you to better understand the natural progression of your illness. With this information you will be encouraged to make decisions regarding your care.
Physician Services: The hospice medical directory, physician employees, and contracted physicians of the hospice, along with your attending physician are responsible for the palliation and management of your terminal illness and any conditions relate to the terminal illness. If your attending physician is not available, the hospice medical director is responsible for meeting your medical needs.
Social Worker: Facing a serious illness can be a time of tremendous pain and confusion for you and your family. Because you must deal with emotions and challenges throughout the time in which the illness is occurring, a social worker may be assigned to help you and your family. Services that may be provided by the social worker include:
- Providing emotional support, counseling and guidance to the patient and family in coping with stress related to the illness;
- Identifying community resources which are available to help you;
- Assisting the patient and family with planning for funeral arrangements, nursing home resources, etc.;
- Offering information about Advance Directives
Hospice Aide: Our hospice aide services are provided under the supervision of a Registered Nurse to patients who have a need for assistance with personal care. Our hospice aides have experience in caring for people in need and have been carefully chosen to provide care. The hospice aide may assist with bathing, hair care, shaving, skin care, linen changes, catheter care, and the patient’s tidying the patient’s immediate surroundings. Hospice aides are not permitted to dispense medications. They will report any changes in the condition of the patient to the Registered nurse.
Physical, Occupational and Speech Therapists: Services are provided by a licensed therapist or therapy assistant under the direction of a therapist. Therapy services may be provided only as reasonable and necessary for symptom control or to enable you to maintain activities of daily living. These services must be approved by the hospice interdisciplinary group and may not be appropriate for all hospice patients.
Volunteers: A vital part of hospice is the carefully selected and well-trained volunteers working alongside the professional staff. These special people provide many different types of support for the hospice program and those coping with terminal illness, grief, and loss. They are good listers, nonjudgmental, adaptable, and have a strong desire to reach out with love and concern to others. Volunteers may be used on a regular schedule or on a call when needed basis.
Spiritual Counselor: Hospice spiritual care is based on a high respect for the patients’ and caregivers’ personal faith and belief. The hospice spiritual counselor is available to assist patients and families cope with the significant spiritual issues that often arise during terminal illness. The services offered include regular pastoral care visits, being on-call and available for crises, conducting funerals and memorial services as requested, and contacting a patient’s own clergy if desired. The spiritual counselor does not impose his/her own beliefs or seek to change the beliefs of the patient or family.
Respiratory Therapist: Care is provided to people with difficulty breathing. This includes assessments and treatment to alleviate shortness of breath and loud or labored breathing. The Respiratory Therapist works with the Registered Nurse and the Physician to ensure that you can breathe easier.
Dietary Counselor: Dietary counseling may be provided by a dietician, nurse or other qualified staff member to address and ensure that your dietary needs are met.
Bereavement: Bereavement services are an integral part of the hospice program. Following a terminal diagnosis, patients and families often struggle with anticipatory grief issues. The medical social worker and spiritual counselor are available to assist families during this emotionally difficult time. Following a hospice patient’s death, hospice continues to provide bereavement support to grieving families. While one individual is identified as the primary contact with the family, generally the spouse or primary caregiver, all members of the family are eligible to receive bereavement services.
These services are available for a period of 13 months following the patient’s death. They include regular mailings to provide support and education regarding grief issues, a grief support group, phone contacts and individual visits as desired by the bereaved. For needs that exceed the scope of hospice bereavement services, referrals to other organizations and professionals within the community are available. These services are also made available to anyone in the community.
Yes. Hospice physicians and team members work with your doctor to ensure your clinical and emotional needs are being met and that your care is being carried out appropriately. Your doctor choose his or her level of participation in your care.
Admission to our hospice program is made upon the recommendation of your physician and is based upon your needs. Normally, appropriate candidates for hospice are patients determined to have a terminal illness (which is defined as having a prognosis of 6 months or less if the disease or illness runs its normal course). You should have a desire for palliative treatment, want to stay at home if possible, and have a primary care person. On admission, our nurse will visit you or your family to discuss hospice services, assess your immediate needs, and recommend a plan of care.
The patient should have an attending physician who is willing to certify the limited life expectancy of the patient, to take care of the medical needs of the patient and to work with the hospice team. It is your right to select your attending physician and we will help you to do this if you do not already have an attending physician.
The patient and attending physician should agree that the goal of treatment under hospice care is palliative in nature, addressing pain and symptom management and is not intended to be curative, life-prolonging or remission-inducing. The patient and primary care person should be informed of the diagnosis and prognosis and give consent for hospice care. You must reside within the service area of the hospice program. Should you move during your hospice benefit, we will help you to locate a hospice near you and work to transfer any helpful information to the new hospice. If we cannot meet your needs either directly or indirectly through service agreements with other providers, we will not admit you or will not continue to provide services for you.
We utilize a plan of care to coordinate your treatments and professionals to meet your identified needs and goals and wishes. The plan includes five basic areas; physical care, personal care and comfort, spiritual needs, psychosocial needs, and bereavement care. The plan is reviewed and updated as needed, based on your changing needs. We encourage your participation and will provide necessary medical information to assist you. You have the right to refuse any medication or treatment procedure. Such refusal may require us to obtain a written statement form you releasing us from all responsibility resulting from such action. Should this happen, we would encourage you to discuss the matter with your physician for advice and guidance.
On admission, you and a clinician will create a list of your current medications (including any over-the counter medications, herbal remedies and vitamins). We will compare this list to the medications ordered by your physician. Our staff will continue to compare the list to the medications that are ordered, administered, or dispensed to you while under our care. This will be done to resolve any discrepancies.
We fully recognize your right to dignity and individuality, including privacy in treatment and in the care of your personal needs. We will always notify you if an additional individual need to be present for your visit for reasons of safety, education, or supervision. Prior to anyone visiting your home, we will ask your permission. You have the right to refuse any visitors and this will not compromise your care in any way.
Routine Home Care: Care is provided intermittently by hospice members in the patient’s or family home or in a nursing care facility.
General Inpatient Care: Care may be provided at a contracted hospital or inpatient hospice facility for patients who need pain control of acute/chronic symptom management which cannot be managed in other settings. The necessity for inpatient and paid length of stay will be determined by the hospice interdisciplinary group. If a hospice patient needs hospitalization for any reason unrelated to the terminal diagnosis, traditional Medicare Part A will be utilized.
Inpatient Respite Care: Up to five (5) days of respite care at a contractual hospital, nursing care facility or inpatient hospice facility will be paid by hospice, if approved by the hospice interdisciplinary group. This benefit may be used to give the family/caregiver a rest and the patient does not need to meet acute care standards.
Continuous Home Care: A minimum of eight (8) hours of care per day may be provided during periods of crisis to maintain the patient at home. Criteria for continuous home care are the same as general inpatient care and consist predominantly of nursing care; however, hospice aides may also supplement nursing care.
No, we understand this is a very personal decision and will respect your right to choose whether or not to have CPR and other resuscitation treatments. We will discuss your choices and make sure that any questions you have are answered honestly.
An advance directive is a legal document that lets you direct in advance the care you will receive at some future time. It is often important near the end of life, when many people are not able to speak for themselves. Completing an advance directive requires that you consider your options and make decisions now, while you are healthy, about what you do and do not want if you are seriously ill and unlikely to get better. Our Social Workers are trained to help you to complete and follow an advanced directive should you desire assistance.
If a patient’s health improves while on hospice care the patient will be evaluated to ensure that hospice is still the right treatment plan. If the patient no longer meets eligibility requirements, we can discharge the patient from hospice and coordinate care that better aligns with his/her goals and wishes.
Selecting a hospice is a difficult decision. The list of questions below may help you to ask questions and make an informed decision.
- Does this provider include clinicians in their senior leadership?
- Does this provider score well on the Hospice Compare website? https://www.medicare.gov/hospicecompare/
- Is this hospice a member of the National Association for Home Care and Hospice or other association to promote excellence in care?
- Is this hospice provider accredited by the Accreditation Commission for Health Care (ACHC) or other reputable accreditation body?
- Does this provider supply literature explaining its services, eligibility requirements, fees, and funding sources? Many providers furnish patients with a detailed “Patient Bill of Rights” that outlines the rights and responsibilities of the providers, patients, and caregivers alike. An annual report and other educational materials also can provide helpful information about the provider.
- How does this provider select and train its employees? Does it protect its workers with written personnel policies, benefits packages, and malpractice insurance?
- Are nurses or therapists required to evaluate the patient’s home care needs? If so, what does this entail? Do they consult the patient’s physicians and family members?
- What specialty positions does this provider have? Do they employ a full time respiratory therapist?
- Does this provider include the patient and his or her family members in developing the plan of care? Are they involved in making care plan changes?
- Is the patient’s course of treatment documented, detailing the specific tasks to be carried out by each professional caregiver? Does the patient and his or her family receive a copy of this plan, and do the caregivers update it as changes occur? Does this provider take time to educate family members on the care being administered to the patient?
- Does this provider assign supervisors to oversee the quality of care patients are receiving in their homes? If so, how often do these individuals make visits? Who can the patient and his or her family members call with questions or complaints? How does the agency follow up on and resolve problems?
- What are the financial procedures of this provider? Does the provider furnish written statements explaining all of the costs and payment plan options associated with home care?
- What procedures does this provider have in place to handle emergencies? Are its caregivers available 24 hours a day, seven days a week?
- How does this provider ensure patient confidentiality?
In addition, ask the home care provider to supply you with a list of references, such as doctors, discharge planners, patients or their family members, and community leaders who are familiar with the provider’s quality of service.
Contact each reference and ask:
- Do you frequently refer clients to this provider?
- Do you have a contractual relationship with this provider? If so, do you require the provider to meet special standards for quality care?
What sort of feedback have you gotten from patients receiving care from this provider, either on an informal basis or through a formal satisfaction survey?
